The Role of TMS in Postpartum Depression Treatment

Caleb Whitenack, MD

For many new mothers, the postpartum period is portrayed as joyful, fulfilling, and full of bonding moments. However, for a significant number of women, this stage also comes with emotional heaviness, confusion, and sometimes, despair. When traditional treatments fall short or aren’t well-tolerated, innovative therapies like Transcranial Magnetic Stimulation (TMS) offer hope—and results.
What Is TMS?
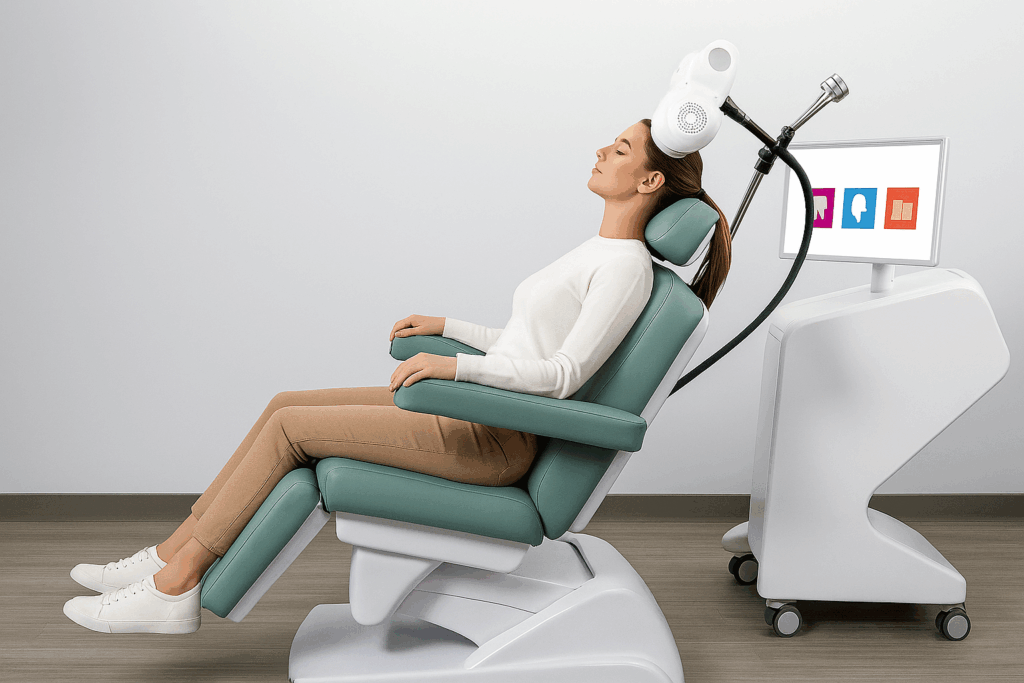
Transcranial Magnetic Stimulation (TMS) is a non-invasive, FDA-approved treatment that uses magnetic pulses to stimulate areas of the brain involved in mood regulation—primarily the prefrontal cortex. Unlike medications, TMS doesn’t circulate through the bloodstream, which means fewer systemic side effects. This makes it an appealing option for individuals who are sensitive to medications or want to avoid pharmacological treatments, particularly in the postpartum phase when breastfeeding may be a concern.
TMS is performed in an outpatient setting. Patients remain awake, and the sessions usually last between 20 and 40 minutes, five days a week over several weeks. Many describe the sensation as tapping on the scalp—uncomfortable at times, but not painful.
Understanding Postpartum Depression
Postpartum depression is more than the “baby blues”. It’s a serious mental health condition that affects an estimated 1 in 7 women, though some studies suggest even higher rates. It typically begins within the first few days to weeks after childbirth but can also develop later in the postpartum year.
Symptoms can include:
- Persistent sadness or tearfulness
- Feelings of hopelessness, guilt, or worthlessness
- Trouble bonding with the baby
- Changes in appetite or sleep
- Intrusive thoughts, images or fears of harming oneself or the baby
The emotional impact can be debilitating—not just for the mother, but also for the child’s development and family dynamic. Early intervention is crucial, but many mothers face barriers to care: stigma, lack of access, fear of medication effects during breastfeeding, and underdiagnosis.
Neurotransmitters Involved in Postpartum Depression
Postpartum depression is rooted in both psychological and biological changes. Hormonal fluctuations play a well-known role, but so do key neurotransmitters in the brain:
- Serotonin: Often referred to as the “feel-good” chemical, serotonin is closely linked to mood stability. Lower levels can be associated with depression and anxiety.
- Dopamine: This neurotransmitter affects motivation, pleasure, and reward. In postpartum depression, disruptions in dopamine function may contribute to feelings of emotional numbness or disinterest in previously enjoyable activities.
- Norepinephrine: Linked to alertness and energy, low norepinephrine may contribute to the fatigue and mental fog many mothers report during PPD.
TMS directly targets the prefrontal cortex, which is involved in regulating these neurotransmitters and others. By stimulating this area, TMS may help rebalance brain activity and restore healthier emotional functioning.
Why Consider TMS for Postpartum Depression?
Traditional treatments for postpartum depression often include psychotherapy and antidepressant medications. While these can be highly effective, they’re not always the right fit for everyone.
Here’s why TMS therapy is gaining traction:
1. Medication-Free Option
Some mothers are hesitant to take antidepressants due to concerns about breastfeeding or side effects. TMS offers a non-pharmacologic treatment path that doesn’t affect milk supply or pass through breast milk.
2. High Success Rates
Clinical studies show that TMS is effective in treating major depressive disorder, including in women with treatment-resistant depression. Many report significant symptom relief after a few weeks of treatment.
3. Minimal Side Effects
The most common side effects of TMS are mild headaches or scalp discomfort. Unlike medications, it doesn’t cause weight gain, sexual dysfunction, or sedation—factors that often make patients discontinue treatment.
4. Functional Recovery
TMS helps not only with mood but also with cognitive clarity, energy, and emotional regulation—all of which are essential for new parents navigating the demands of early parenthood.
Is TMS Safe During the Postpartum Period?

Safety is a key concern for any postpartum intervention. The good news? TMS is non-invasive, non-sedative, and has a strong safety profile. It doesn’t require hospitalization or downtime and has no known effects on hormonal balance or infant health.
Of course, it’s important that postpartum women consult with a psychiatrist experienced in TMS to evaluate individual risk factors and determine the best course of action.
Final Thoughts
Postpartum depression can be isolating and overwhelming. But it’s not a reflection of your worth or your ability to parent—it’s a medical condition, and it’s treatable.
TMS therapy offers a path forward that’s grounded in science and compassion. For mothers who feel like they’ve exhausted their options—or who are looking for something that works without adding to their emotional or physical burden—TMS can be a powerful part of healing.
Responsibly edited by AI
Other Blog Posts in
Animo Sano Psychiatry is open for patients in North Carolina, Georgia and Tennessee. If you’d like to schedule an appointment, please contact us.
Get Access to Behavioral Health Care
Let’s take your first step towards. Press the button to get started. We’ll be back to you as soon as possible.ecovery, together.




