Trauma leaves an indelible mark on the brain. However, through the incredible phenomenon of neuroplasticity, the brain has the power to adapt, heal, and rewire itself. Coupled with Cognitive Behavioral Therapy (CBT), neuroplasticity offers hope and actionable pathways for individuals seeking recovery from trauma.
The Impact of Trauma on the Brain
Trauma profoundly affects the brain’s structure and function. Chronic exposure to traumatic events can shrink the hippocampus, responsible for memory and learning, and over activate the amygdala, which governs fear responses. Simultaneously, the prefrontal cortex, essential for decision-making and emotional regulation, may become less active. These changes contribute to the symptoms of PTSD, anxiety, and depression often observed in trauma survivors.
Studies reveal that these alterations in brain structure are not permanent. Neuroplasticity, the brain’s ability to reorganize itself by forming new neural connections, provides a foundation for recovery. This adaptability is the cornerstone of neuroplasticity therapy and neuroplasticity treatment, which aim to restore balance and functionality to the brain.

What is Neuroplasticity?
Neuroplasticity refers to the brain’s capacity to adapt to new experiences, learn new skills, and recover from injuries. When it comes to trauma, neuroplasticity underscores the brain’s potential to heal from the negative impacts of distressing experiences. Activities that stimulate neuroplasticity, such as mindfulness practices, physical exercise, and structured therapy, create new neural pathways and strengthen existing ones.
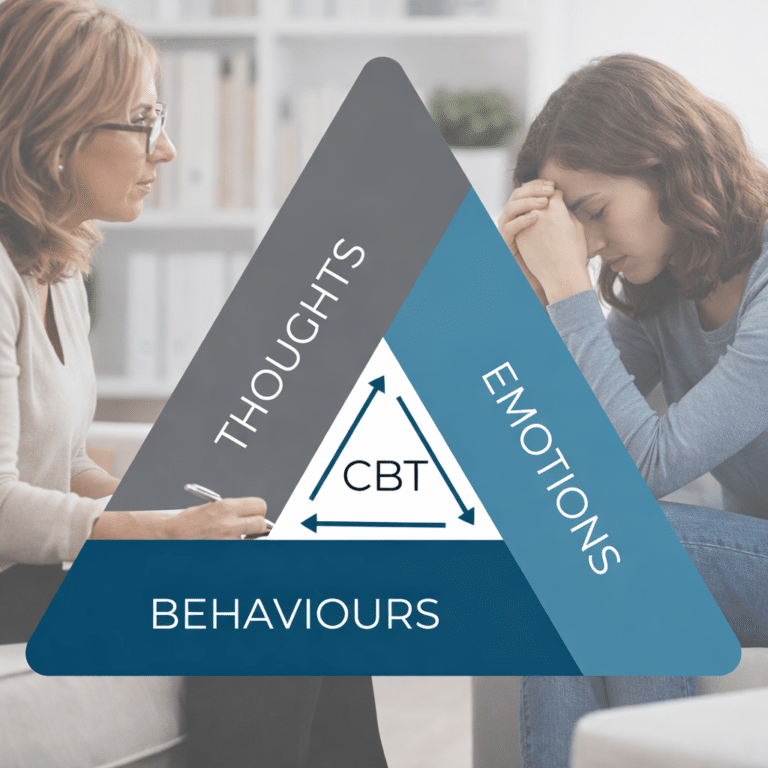
Cognitive Behavioral Therapy and Neuroplasticity
CBT is a gold-standard approach to treating trauma-related disorders. By challenging negative thought patterns and replacing them with healthier perspectives, CBT directly influences how the brain processes emotions and memories. Research shows that CBT for trauma fosters neuroplasticity by encouraging the brain to form new, positive associations. For example:

- Repeatedly challenging irrational beliefs can rewire pathways in the prefrontal cortex, enhancing logical reasoning.
- Exposure therapy, a key element of CBT, can help diminish the amygdala’s overactivity by reducing fear responses over time.
Integrating CBT with neuroplasticity-focused practices creates a powerful synergy. Techniques like journaling, mindfulness, and visualization amplify therapy’s effectiveness, accelerating the brain’s healing process.
How Neuroplasticity and CBT Work Together to Heal Trauma
- Reframing Negative Thought Patterns: Trauma often ingrains unhelpful beliefs, such as “I am unsafe” or “I am unworthy.” CBT encourages reframing these thoughts, prompting the brain to create alternative, healthier neural pathways.
- Strengthening Emotional Regulation: Emotional dysregulation is a common aftermath of trauma. CBT enhances the brain’s capacity to regulate emotions by stimulating the prefrontal cortex, fostering better control over reactions.
- Promoting Exposure and Desensitization: Avoidance behaviors can perpetuate fear. Exposure therapy, a component of CBT, gradually reduces fear responses, demonstrating the brain’s ability to “unlearn” maladaptive reactions.
- Facilitating Memory Processing: Trauma memories can feel fragmented and overwhelming. CBT helps individuals process and integrate these memories, reducing their emotional intensity and allowing for closure.
Evidence Supporting Neuroplasticity and CBT
Scientific evidence underscores the transformative potential of neuroplasticity and Cognitive Behavioral Therapy (CBT). A study published in The Journal of Pain revealed that an 11-week CBT intervention for chronic pain resulted in increased gray matter volume in the prefrontal cortex, enhancing decision-making and emotional regulation. Another study highlighted that individuals undergoing CBT for post-traumatic stress disorder (PTSD) experienced significant changes in amygdala connectivity with the fronto-parietal network, correlating with decreased symptoms.
Final Thoughts
The brain’s ability to heal is a testament to its resilience and adaptability. Trauma may reshape the brain, but Neuroplasticity and CBT offer pathways to recovery, enabling individuals to reclaim control over their lives. By understanding the intricate relationship between trauma, neuroplasticity, and therapy, we empower ourselves to pursue healing and growth.
Responsibly edited by AI
Animo Sano Psychiatry is open for patients in North Carolina, Georgia and Tennessee. If you’d like to schedule an appointment, please contact us.
Get Access to Behavioral Health Care
Let’s take your first step towards. Press the button to get started. We’ll be back to you as soon as possible.ecovery, together.