As someone deeply immersed in the realm of psychiatry, I’ve come to recognize the profound importance of collaborative care in mental health treatment. This effective approach brings together a cohesive team of professionals, each bringing their unique skills to the table for the benefit of the patient. Why, you might ask, is this so essential in mental health therapy? Walk with me, dear reader, as we delve into this crucial topic.
Picture this—you are standing in the middle of a bustling city, lost and confused. You’re trying to navigate through endless roads and bylanes leading to various destinations. If you had the assistance of locals hailing from different parts of the city, each contributing with their unique knowledge of the place, wouldn’t it make your journey a lot simpler? This, in essence, is akin to the ideology behind the Collaborative Care Model.
The absolute beauty of the Collaborative Care Model is its team-based approach. When psychiatrists, psychologists, nurses, social workers and other healthcare professionals jointly come together offering their insights, it is like a symphony of healing for patients dealing with mental health challenges. I can’t stress enough the value this holistic perspective brings to mental health treatment. When different professionals examine the issue through their distinct lenses, the patient is offered a bird’s eye view of their mental health and provided with a comprehensive treatment plan, tailored specifically for them. Yikes! Doesn’t that sound like a supercharged experience in healing?

The approach doesn’t just stop with providing qualitative treatment. It’s no secret that the conventional route to seeking mental health aid has been a laborious one. Accessing specialists comes with its own tedious timeline, often leading to delays in diagnosis and treatment. The Collaborative Care Model offers a dynamic solution to this—by providing an all-inclusive solution, it significantly improves access to specialized aid, and in turn, propels patients faster onto their path of recovery.
Economic growth and workforce productivity also benefit indirectly from this model. Frequent emergency visits and outpatient psychiatric services often lead to skyrocketing healthcare costs. Collaborative Care Models have been proven to minimize these unnecessary expenses while maximizing the patient’s wellbeing. Besides, when patients receive efficient, high-quality treatment, their personal involvement in society and the workplace naturally improves, leading to overall economical and social growth.
Important to note is that this approach isn’t just a fancy hypothesis. It’s well-founded, has countless success stories and often reimbursable by various insurance providers such as Medicare, BCBS, among others. Well, if it is a shift in the right direction, well-supported and cost-effective, the question isn’t why we should adopt Collaborative Care, but rather why we haven’t embraced it more fully already? I can’t help but ponder.
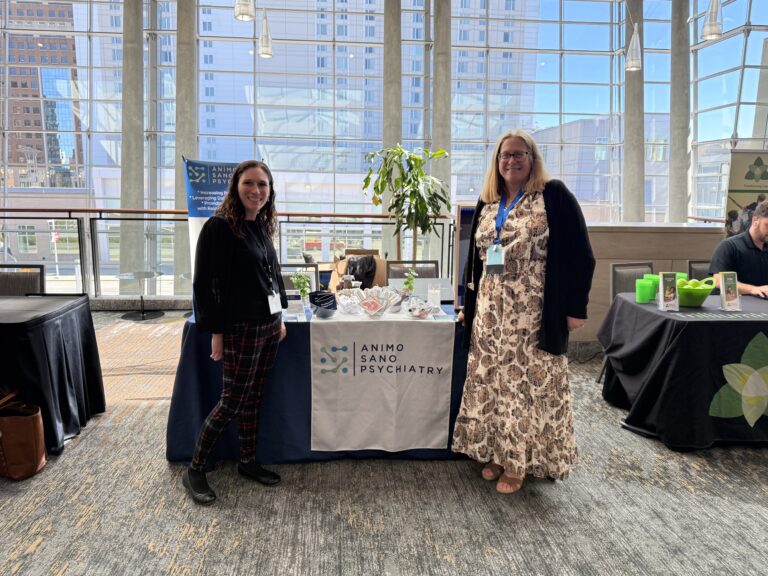
Finally, let’s hear it straight from the horse’s mouth. At Animo Sano Psychiatry, our Collaborative Care Director, Jennifer Street, and Medical Director, Mina Boazak, MD, have firsthand experience of the immense potential this model holds. According to them, it’s akin to a power-packed rally of experts, working relentlessly to uplift patients from the ditches of mental health adversities. You see, at the end of the day, it’s all about ensuring wellness is a collective triumph and not a solitary struggle.
In conclusion, the virtues of Collaborative Care Model in mental health treatment can’t be overemphasized. It’s not just about healing the mind, it’s about healing the community, the society and the heart of productivity—the workforce. It’s now time we acknowledged and heralded the collaborative effort as the new beacon of mental wellness. Now that’s worth striving for.
Responsibly edited by AI
Other Blog Posts in
Animo Sano Psychiatry is open for patients in North Carolina, Georgia and Tennessee. If you’d like to schedule an appointment, please contact us.
Get Access to Behavioral Health Care
Let’s take your first step towards. Press the button to get started. We’ll be back to you as soon as possible.ecovery, together.