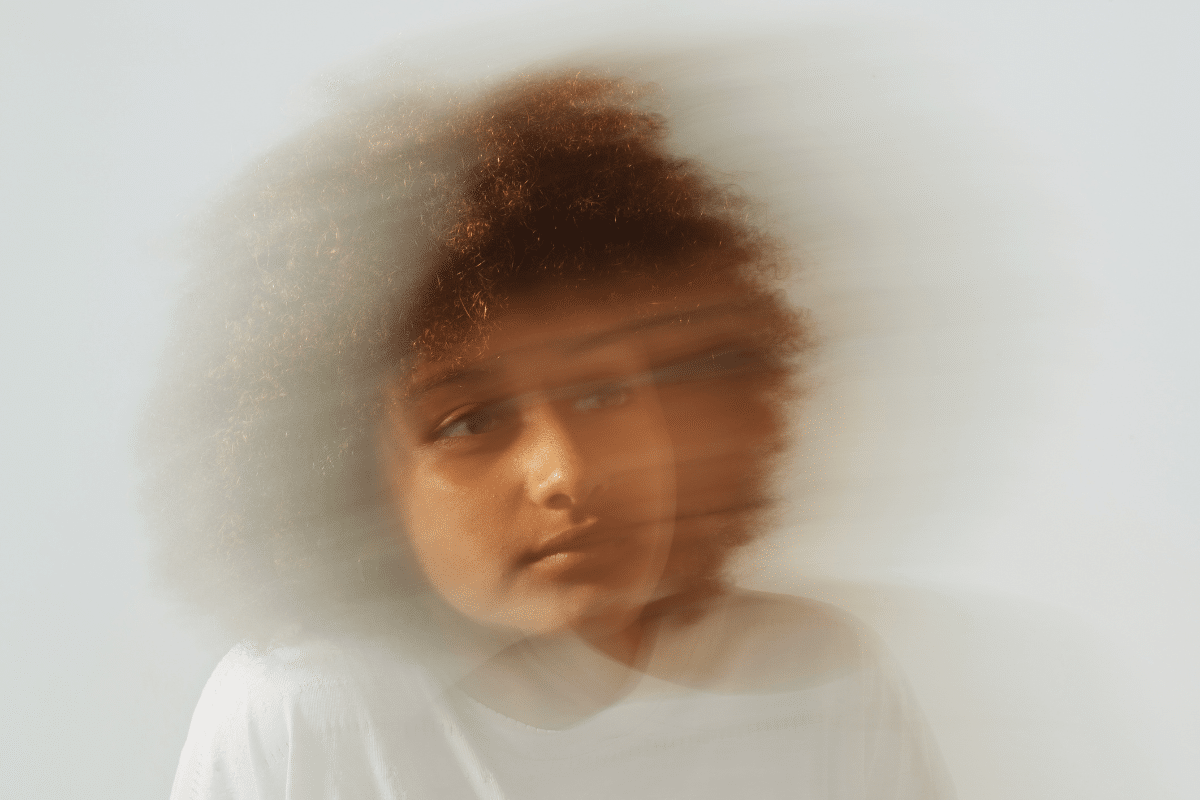
Depression is a broad term that encompasses a range of mood disorders, but not all depressions are the same. One of the most biologically rooted and severe subtypes is Melancholic Depression—now recognized in clinical psychiatry not as a standalone diagnosis, but as a specifier of Major Depressive Disorder (MDD) in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Unlike other forms of depression that may temporarily improve in response to positive events, melancholic depression is defined by a pervasive lack of pleasure and emotional reactivity regardless of external circumstances.
What Sets Melancholic Depression Apart?
Melancholic depression is distinguished by symptoms that are often more biologically driven than situational. Rather than being a reaction to external stress, it manifests through “somatic” or physical symptoms. Those experiencing it often face a ‘flatness’ that follows a rigid rhythm, where physical functioning and mood are dictated by internal biological shifts rather than what is happening in the world around them
Key Clinical Features
- Anhedonia: The inability to experience pleasure in nearly all activities—even those that were once enjoyed.
- Lack of Emotional Reactivity: Positive events do not improve mood—even temporarily—differentiating melancholia from other depressive subtypes like atypical depression.
- Distinct Quality of Depressed Mood: Patients often describe a profound emptiness or heaviness that is qualitatively different from ordinary sadness.
- Diurnal Variation: Symptoms are typically worst in the morning, with slight involuntary improvement as the day progresses.
- Psychomotor Disturbances: Changes in physical movement, including retardation (slowed speech and movement) or agitation (restless pacing or hand-wringing), are common.
- Early Morning Awakening: Individuals often wake at least two hours earlier than usual with intense dread or anxiety.

The Biological Foundations
A defining characteristic of melancholic depression is its biological autonomy—the symptoms persist independently of life events or environmental influences once an episode begins.
Neurobiological Disruption:
Melancholic patients often show disruptions in the Hypothalamic-Pituitary-Adrenal (HPA) axis, the body’s central stress response system. This dysregulation commonly leads to elevated cortisol levels and altered circadian rhythms, which are linked with mood severity and biological markers of depression.
Sleep Architecture Alterations
In melancholic depression, sleep patterns are distinctly altered:
- Reduced REM latency (entering REM sleep more quickly than typical)
- Decreased deep, restorative slow-wave sleep
- Early morning awakening and fragmentation of sleep cycles
These changes are strongly tied to dysregulated HPA activity and contribute to chronic fatigue and cognitive difficulties.
Evidence-Based Treatment Approaches

Due to its robust biological underpinnings, melancholic depression often responds best to clinical medical treatments.
Medication
While SSRIs (Selective Serotonin Reuptake Inhibitors) are commonly prescribed for depression, melancholic depression often shows better response to medications that target multiple neurotransmitter systems such as:
- SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors)
- Tricyclic Antidepressants (TCAs)
These have a broader impact on both serotonin and norepinephrine pathways.
Electroconvulsive Therapy (ECT)
In severe or treatment-resistant cases, ECT remains one of the most effective interventions, with high rates of rapid symptom remission. Clinical guidelines still consider ECT a standard of care for melancholic features that are severe or unresponsive to medication.
Structured Circadian Routine
Because symptoms follow a daily rhythm, maintaining a strict routine with:
- Regular, consistent sleep and wake times
- Morning light exposure
- Scheduled activity
can help stabilize internal biological clocks and complement medical interventions.
Final Thoughts
Melancholic depression is not a reflection of personal weakness or lack of resilience—it is a serious clinical condition rooted in physiological changes. It represents a literal shift in how the brain and body function at a systemic level. Recognition of its distinctive symptoms—such as pervasive anhedonia, symptoms are worse in the mornings, psychomotor changes, and lack of emotional reactivity—helps clinicians tailor interventions that target its biological rather than psychosocial drivers.
With accurate diagnosis and evidence-based treatment, many individuals with melancholic depression can experience meaningful recovery.
Frequently Asked Questions (FAQs)
1. How does melancholia differ from atypical depression?
In atypical depression, mood can improve temporarily in response to good events—a feature known as mood reactivity. In melancholic depression, mood remains flat and unresponsive to positive stimuli.
2. Can a sad life event cause melancholic depression?
While a stressor can trigger an episode, once melancholia develops, its persistence is largely biologically driven and independent of external events.
3. Is melancholia a permanent condition?
No. It is episodic. Many patients achieve full remission with targeted biological treatments.
4. Why are symptoms worse in the morning?
This pattern relates to the body’s circadian rhythms and dysregulated cortisol peaks in melancholic depression.
Responsibly edited by AI
Other Blog Posts in
Animo Sano Psychiatry is open for patients in North Carolina, Georgia and Tennessee. If you’d like to schedule an appointment, please contact us.
Get Access to Behavioral Health Care
Let’s take your first step towards. Press the button to get started. We’ll be back to you as soon as possible.ecovery, together.





