What Is Dual Diagnosis? Understanding the Overlap Between Mental Health and Substance Use

Jasmine Zaman
Mental health and substance use are often treated as separate issues, but in reality, they frequently go hand-in-hand. When someone experiences both a mental health disorder and a substance use disorder simultaneously, it’s referred to as “dual diagnosis” or “co-occurring disorders.” This overlap presents unique challenges, but with the right understanding and care, recovery is entirely possible.
What is Dual Diagnosis?
Dual diagnosis occurs when a person is affected by both a mental illness and a substance use disorder. This doesn’t just mean the two happen to exist in the same person; they often interact in complex and reinforcing ways. For example, someone struggling with anxiety may begin using alcohol to self-medicate. Over time, the alcohol use might worsen the anxiety, creating a cycle that becomes hard to break.
Some of the most commonly seen combinations include:
- Depression and alcohol use disorder
- Anxiety disorders and benzodiazepine misuse
- Bipolar disorder and stimulant abuse
- PTSD and opioid addiction
- Schizophrenia and cannabis use disorder
The interaction between these conditions often makes diagnosis and treatment more difficult. Mental health symptoms may mask substance use, and vice versa. Moreover, substance use can exacerbate psychiatric symptoms or trigger them in someone who is already vulnerable. This makes comprehensive assessment crucial in identifying both issues.
According to AddictionGroup.org, “Over 9 million U.S. adults have experienced both a substance use disorder and a mental illness in the past year,” and “Recent estimates from federal health surveys suggest that 9 to 10 million adults annually have both a substance use issue and a co‑existing mental health condition”

Dual Diagnosis Treatment
Treating dual diagnosis effectively requires an integrated and holistic approach. Traditional models often attempted to treat mental health and substance use issues separately, sometimes requiring individuals to achieve sobriety before beginning mental health treatment. However, research has shown that addressing both conditions simultaneously leads to better outcomes.
Integrated Treatment Model
Integrated treatment brings mental health and substance use specialists together as one care team, ensuring both conditions are addressed in sync. Key elements include:
- Comprehensive Assessment: A thorough review of mental health and substance use history using structured tools.
- Medication Management: With close monitoring, medications may be used to stabilize mood or manage cravings.
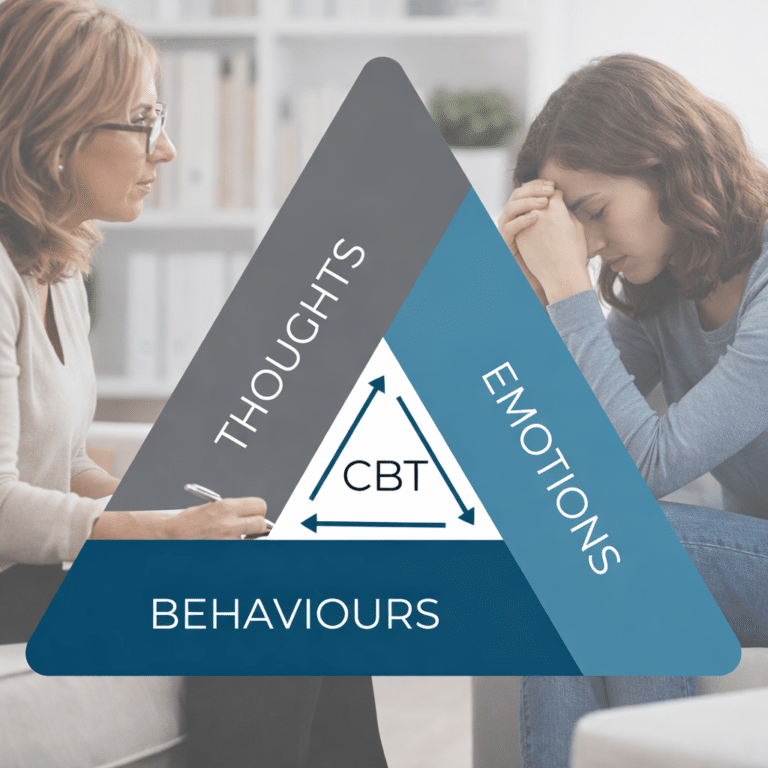
- Evidence-Based Therapies: Approaches like CBT (Cognitive Behavioral Therapy), DBT (Dialectical Behavior Therapy), and MI (Motivational Interviewing) help build coping skills and reduce harmful behaviors.
- Relapse Prevention: Plans address triggers for both mental health symptoms and substance use.
- Peer & Social Support: Group therapy, peer programs, and family involvement strengthen recovery.
- Continuum of Care: Long-term support ensures ongoing stability through outpatient services and community resources.
Integrated care goes beyond symptom relief—it helps people reconnect with themselves and build a life rooted in purpose and stability.
What Is an Example of Dual Diagnosis?

To understand dual diagnosis more clearly, consider the following scenario:
Sarah is a 28-year-old woman who has struggled with anxiety since her teenage years. In college, she found that drinking alcohol helped her feel more relaxed in social situations. Over time, her alcohol use increased to the point where she was drinking daily that resulted in causing substance use disorder. She started missing work, and her relationships became strained. She felt ashamed and isolated but couldn’t seem to stop. When she finally sought help, it became clear that she wasn’t just dealing with alcoholism—her underlying anxiety was driving much of her behavior.
In Sarah’s case, both the anxiety and the alcohol use needed to be addressed for her to fully recover. Simply stopping alcohol use without treating the anxiety would leave her vulnerable to relapse. Similarly, treating the anxiety without helping her manage cravings and build sobriety skills wouldn’t be effective.
Final Thoughts
Dual diagnosis is more common than many realize, and yet it’s often misunderstood. It requires compassion, expertise, and a willingness to look beyond symptoms to the whole person. Recovery is not only possible, it’s expected when care is coordinated and person-centered.
If you or someone you love is struggling with both mental health and substance use challenges, know that help is available. You don’t have to choose which problem to tackle first. With the right support, you can heal both.
Responsibly edited by AI
Other Blog Posts in
Animo Sano Psychiatry is open for patients in North Carolina, Georgia and Tennessee. If you’d like to schedule an appointment, please contact us.
Get Access to Behavioral Health Care
Let’s take your first step towards. Press the button to get started. We’ll be back to you as soon as possible.ecovery, together.