Understanding the Bipolar Spectrum: The Brain’s Role in Mood Swings and Mania

Jasmine Zaman

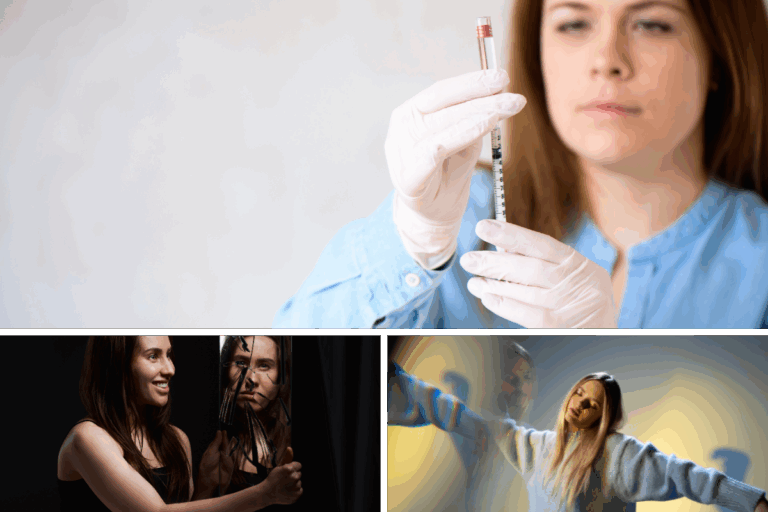
Bipolar spectrum disorders are complex mental health conditions that involve recurring shifts in mood, energy, and activity levels. These shifts can range from episodes of elevated mood and increased activity—known as mania or hypomania—to periods of deep sadness, fatigue, and loss of interest, characteristic of depression. While often misunderstood as simply “moodiness,” bipolar disorder reflects underlying neurological changes that impact how the brain processes emotion, motivation, and impulse control. Recognizing these biological roots is essential to both accurate diagnosis and effective treatment.
The Neuroscience Behind Bipolar Disorder
When we talk about the neuroscience behind bipolar disorder, we’re referring to tangible, measurable changes in the brain. Imaging studies consistently find differences in areas like the prefrontal cortex (crucial for decision‑making), the amygdala (where emotion is processed), the hippocampus (memory), and the anterior cingulate cortex (regulating conflict and emotional control). These areas don’t live in isolation—they form a network. And when that network is wired differently, mood regulation gets disrupted.
On the chemical side, the brain’s “language” relies on neurotransmitters like dopamine, serotonin, glutamate, and GABA. In bipolar disorder, dopamine tends to spike during manic episodes—fueling impulsivity, racing thoughts, and euphoric highs—then crash during depressive phases . Too much glutamate activity may trigger excitability and even toxicity, while lower GABA levels limit the brain’s ability to apply emotional “brakes.”
And there’s more—right down at the gene-expression level. Variations and epigenetic changes (such as DNA methylation in clock genes and serotonin transport genes) can reshape how these neurochemical systems function.

How Do Mood Swings Develop?
Understanding how mood swings develop helps us see why symptoms aren’t random—they’re patterned.
1. Genes and Life’s Stressors
Bipolar disorder has strong heritability—twin studies suggest up to 80% of risk can be inherited. Genes affecting calcium channels and neurotransmitter regulation are often involved. But environment matters too—trauma, sleep deprivation, or chronic stress can leave epigenetic marks that influence brain circuits long-term.
2. Circuitry in Flux
When connections between emotion-processing areas (like the amygdala) and control regions (like the prefrontal cortex) weaken, mood regulation falters. That’s where the ups and downs begin. One moment, impulse control is overridden; the next, depressive regulation overshoots.
3. The Effects of Time
Over months and years, repeated episodes can physically reshape the brain. MRI scans show gradual loss of gray matter in frontal and limbic regions—a type of neural wearing—making emotional control even more challenging if left untreated.
What Role Does the Brain Play in Bipolar Disorder?
The brain’s influence isn’t just chemical or structural—it’s rhythmic and bioenergetic too.
Neural Circuit Activation
During manic episodes, reward circuits (like the nucleus accumbens) are excitable—and the prefrontal cortex’s ability to regulate them is muted. That’s why you might hear of risky financial decisions, racing thoughts, or hypersexuality in mania. Conversely, depression reflects a dampening of these circuits and poorer regulation from control centers.
The Clock Genes
Our brains follow internal rhythms—sleep, energy, even when our neurotransmitters fire. Genes like CLOCK and BMAL1 are central to these rhythms. When these clocks are out of sync—common in bipolar disorder—dopamine firing patterns can shift, increasing vulnerability to both mania and depression. Interventions like stabilizing sleep—and timing light exposure—can help re-align these rhythms.
Cellular Stress and Mitochondria
Brain cells under oxidative stress or mitochondrial strain are more susceptible to dysfunction. Studies link bipolar disorder to mitochondrial irregularities and oxidative cell damage. Medications like lithium don’t just regulate mood—they also support mitochondrial health, reduce oxidative stress, and protect the brain over time.
Bringing It All Together

Bipolar disorder isn’t a character flaw—it’s the result of a brain that’s wired, weighted, and wired again in ways that challenge emotional regulation. It shows us just how intertwined our brain’s structure, chemistry, rhythms, and energy systems really are.
Treatment needs to be equally multifaceted:
- Medication (e.g., lithium, anticonvulsants, mood stabilizers) supports balance and protects brain health.
- Therapy and structure—from CBT to daily routines—help stabilize sleep, identify stress triggers, and build coping strategies.
- Early, continuous care preserves neuroplasticity and reduces the risk of progressing damage.
Final Thoughts
Bipolar spectrum disorders reflect complex interactions between brain structure, neurochemistry, genetics, and environmental stressors. Research continues to confirm that these conditions are rooted in measurable neurological differences—impacting areas of the brain responsible for emotion, decision-making, impulse control, and circadian rhythm regulation.
Understanding these biological underpinnings allows for more targeted and compassionate treatment approaches. Recognizing the brain’s role in bipolar disorder is key to reducing stigma and encouraging early, sustained care.
Responsibly edited by AI
Other Blog Posts in
Animo Sano Psychiatry is open for patients in North Carolina, Georgia and Tennessee. If you’d like to schedule an appointment, please contact us.
Get Access to Behavioral Health Care
Let’s take your first step towards. Press the button to get started. We’ll be back to you as soon as possible.ecovery, together.