Supporting the Mental Health of Primary Care Providers: How Collaborative Care Benefits Clinicians’ Well-being
Jennifer Street

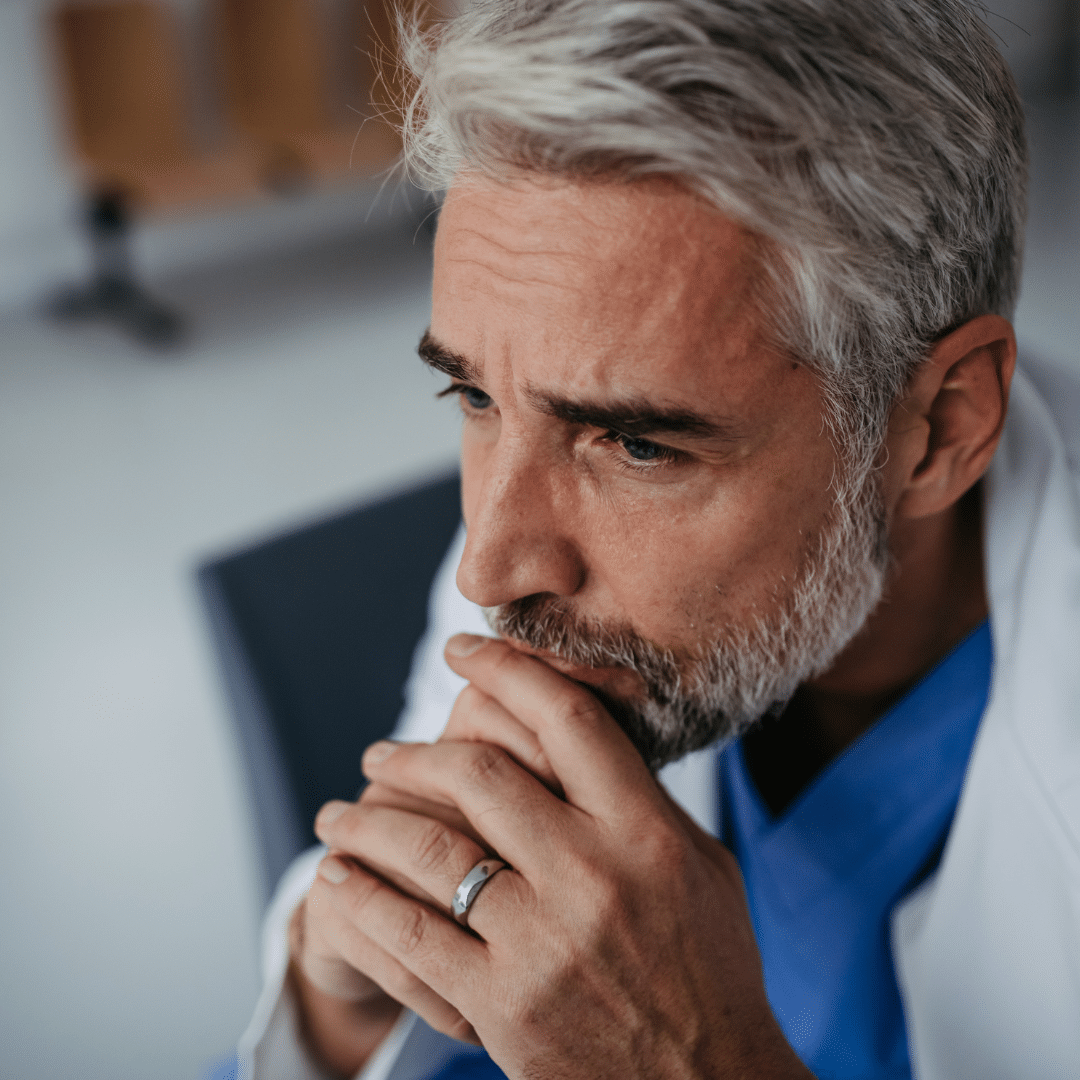
Primary care providers (PCPs) are the heroes of our healthcare system. They’re often the first to see patients, tackling everything from routine check-ups to complex medical conditions. But this crucial role comes with immense pressure, which can take a toll on their mental health. Burnout, anxiety, and depression are all too common among PCPs, impacting the quality of care they provide. This is where the collaborative care model comes into play, offering a supportive framework that can greatly enhance the well-being of clinicians.
The Mental Health Challenges Faced by Primary Care Providers
Being on the front lines of healthcare is no small feat. PCPs deal with a high volume of patients and a diverse range of medical issues daily. This constant demand can lead to significant stress and burnout. According to a 2019 study, nearly 44% of physicians reported experiencing burnout symptoms. Burnout doesn’t just affect providers; it also diminishes the quality of care patients receive.
What is Collaborative Care?
Collaborative care is an integrated approach that brings together primary care providers, mental health specialists, and other healthcare professionals to offer comprehensive patient care. This model emphasizes teamwork, shared decision-making, and coordinated treatment plans. Unlike traditional care models, collaborative care fosters a supportive environment where PCPs are not alone in managing the complex needs of their patients.
How Collaborative Care Benefits Clinicians

1. Reducing Burnout
The collaborative care model spreads the workload among a team of healthcare professionals, easing the individual burden on PCPs. By sharing responsibilities, providers can focus on their strengths and expertise, reducing stress and preventing burnout. In 2016, a study found that collaborative care interventions led to significant improvements in clinician well-being and reduced burnout symptoms.
2. Creating a Supportive Network
Collaborative care fosters a supportive network for PCPs, offering regular opportunities for case discussions and peer support. These interactions provide emotional relief and professional guidance, helping clinicians feel less isolated. With mental health specialists on the team, PCPs have immediate access to expert advice, which can be incredibly reassuring.
3. Improving Patient Outcomes
When PCPs work within a collaborative care model, patient outcomes improve significantly. This, in turn, boosts morale and job satisfaction for clinicians. Knowing they’re providing high-quality, effective care can be a powerful antidote to feelings of inadequacy and stress. The American Psychological Association highlighted that collaborative care models lead to better patient outcomes, contributing positively to clinician satisfaction.
4. Access to Mental Health Resources
In a collaborative care setting, PCPs have direct access to mental health resources and specialists. This access is crucial for timely consultations and support, allowing PCPs to address mental health concerns more effectively. It also means that PCPs themselves can benefit from these resources, ensuring their mental health needs are met.
5. Better Work-Life Balance
Collaborative care promotes a healthier work-life balance for PCPs by encouraging team-based care and shared responsibilities. This approach allows clinicians to manage their workload more effectively and take necessary breaks, which is essential for maintaining mental health. Studies show that healthcare providers in collaborative settings report better work-life balance and higher job satisfaction.
Final Thoughts
Supporting the mental health of primary care providers is crucial for the overall effectiveness of the healthcare system. The collaborative care model offers a promising solution by creating a supportive, integrated environment that benefits clinicians and patients. By reducing burnout, enhancing support, and improving patient outcomes, collaborative care ensures that PCPs can thrive and provide the best possible care.
Responsibly edited by AI
Other Blog Posts in
Animo Sano Psychiatry is open for patients in North Carolina, Georgia and Tennessee. If you’d like to schedule an appointment, please contact us.
Get Access to Behavioral Health Care
Let’s take your first step towards. Press the button to get started. We’ll be back to you as soon as possible.ecovery, together.