
Photo by Ben Blennerhassett on Unsplash
Sleep disorders, such as insomnia and nightmares, are common in post-traumatic stress disorder (PTSD). In this article we will talk about PTSD-related sleep disorders and their treatment.
Relationship between sleep disorders and trauma
Scientific evidence indicates that sleep is necessary to transform a traumatic experience into a less threatening memory and therefore promotes resilience. When a person experiences a traumatic event of catastrophic magnitude, their chances of developing sleep disorders, and even PTSD increase, and if they already suffered from a sleep disorder beforehand, the risk of developing PTSD is even greater.

Photo by Alexandra Gorn on Unsplash
PTSD-related sleep disorders include insomnia and nightmares. Among the common symptoms of PTSD, is a state of hypervigilance. This consists of increased reactivity to the surrounding environment, which can interferewith the individual’s ability to fall asleep and increases the number of awakenings during the night. Nightmares, on the other hand, lead to avoidance of sleep for fear of re-experiencing the trauma. This can create a vicious cycle that worsens the patient’s condition.
PTSD-related insomnia
Insomnia affects anywhere between 30 and 64% of people with PTSD. It can be asecondary symptom to the state of hypervigilance as discussed above. This can affect both the individual’s ability to fall asleep and may increase the number of awakenings during the night.
People with PTSD resort to compensatory behaviors such as leaving the light or TV on all night or using substances to stay alert during the day, all of which ultimately worsen insomnia.
Post-traumatic nightmares
Nightmares may be a part of the intrusive symptoms of PTSD. They usually begin as trauma-related distressing dreams and can progress in intensity to nightmares where often,the original trauma is re-experienced.
While non-traumatic nightmares occur during the second half of the night in REM sleep episodes (the stage of sleep during which we dream), post-traumatic nightmares can occur throughout the night in both REM and non-REM sleep episodes.

Photo by Glen Hodson on Unsplash
The severity of nightmares results insome people trying to avoid falling asleep and may then result inincreased alertness at night due to the feeling of vulnerability associated with this form of reviviscence.
Comorbid sleep disorders in PTSD
In addition to insomnia and nightmares, PTSD is associated with a high incidence of other comorbid sleep disorders. The most frequently diagnosed PTSD comorbid sleep disorders are:
- Sleep-related breathing disorder (SRBD) such as obstructive sleep apnea (OSAS) and upper airway resistance.
- REM sleep behavior disorder (RBD)
- Nocturnal panic attacks
- Sleep terror
- Periodic limb movement disorder (PLMD)
The quality and quantity of sleep during the night can predict the intensity of PTSD symptoms during the following day. Essentially, the more severe the sleep disorders, the more severe the symptoms of PTSD during the day. Hence the treatment of trauma-related sleep disorders and other comorbid sleep disorders is a relevant objective in the approach to people with PTSD.

PTSD-related sleep disorders treatment
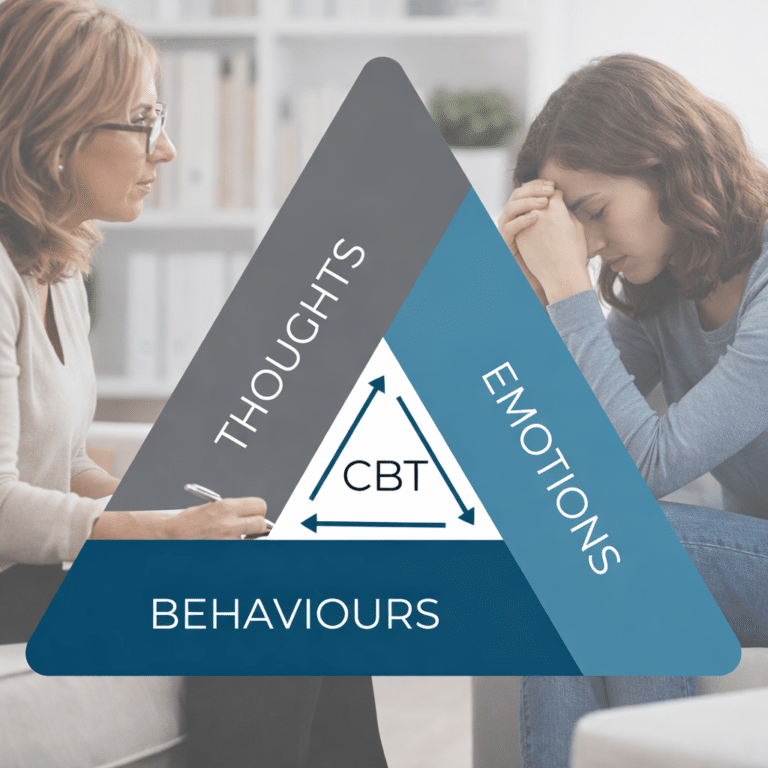
PTSD-related sleep disorders have specific therapeutic options with which it is possible to return to restful sleep and improve PTSD symptoms. Treatment should combine a psychotherapeutic approach with supportive pharmacological treatment.
Psychotherapeutic treatment

Cognitive behavioral therapy for insomnia (CBT-I) is the psychotherapy of choice for chronic insomnia and also the preferred approach to PTSD-related insomnia. Although CBT-I is a disorder-specific therapy that must be administered by a professional trained in this technique, there are additional resources that serve as support for the implementation of what has been learned during the sessions with your health provider like the CBT-I Coach mobile app from the National Center for PTSD.
In the case of post-traumatic nightmares Imagery Rehearsal Therapy (IRT) is the psychotherapy of choice.

IRT consists of modifying the nightmare so it gradually become less stressful and eventually disappear. The patient “rewrites” the scenes, replacing the threatening images with positive ones. The new images should be rehearsed throughout the day so that the new content appears in the dreams.
There are other psychotherapeutic alternatives used as a complement to those mentioned. A specialist can help design the combination of psychotherapeutic techniques that best suits each particular case.
Pharmacological Treatment
Currently, the scientific evidence supporting pharmacological treatment for sleep disorders in PTSD is limited; however, there are some medications that have proven to help. Prazosin, an antihypertensive, is commonly used to help decrease the frequency and severity of nightmares. Other options to help with insomnia may include antidepressants (e.g. mirtazapine, trazodone) and sedative atypical antipsychotics (e.g. quetiapine).
Patients with PTSD may have an increased risk of developing dependency to drugs such as benzodiazepines and “Z drugs” (zolpidem, zopiclone), therefore, these are typically used short-term or after other treatment options have failed.
Other Blog Posts in
Animo Sano Psychiatry is open for patients in North Carolina, Georgia and Tennessee. If you’d like to schedule an appointment, please contact us.
Get Access to Behavioral Health Care
Let’s take your first step towards. Press the button to get started. We’ll be back to you as soon as possible.ecovery, together.